Addison’s disease is a rare endocrine disorder that often goes unnoticed. It shows symptoms that seem like common health issues but actually point to a deeper problem with hormone balance. An Addison’s disease overview shows it as a chronic condition where the adrenal glands don’t make enough important hormones.
This disease comes from the body’s immune system attacking healthy tissue. This is a sign of how complex our internal systems are. Addison’s disease causes ongoing fatigue and other symptoms that might seem like minor problems.
Understanding Addison’s disease is more than just knowing its symptoms. It’s about seeing how it affects people’s lives every day. This guide aims to help those facing this condition by offering support and understanding.
Key Takeaways
- Grasping the intricacies of Addison’s disease is essential for accurate diagnosis and management.
- Adrenal insufficiency can significantly disrupt an individual’s health and daily functioning.
- Autoimmune mechanisms represent a primary cause behind the development of Addison’s disease.
- Early identification of symptoms contributes to better outcomes and improved quality of life for patients.
- Information empowers individuals to advocate for their health in the face of rare conditions like Addison’s disease.
Understanding Addison’s Disease and Its Impact on Health
Addison’s disease is a condition where the adrenal glands don’t work right. This leads to a lack of important hormones. The main ones affected are cortisol and aldosterone, which are key for many body functions.
The Basics of Addison’s Disease
The adrenal glands play a vital role in making hormones. These hormones help control many body processes. Addison’s disease happens when the adrenal cortex doesn’t work well. This causes a lack of cortisol and aldosterone.
This imbalance affects how the body handles stress and keeps a healthy metabolism.
How Addison’s Disease Affects the Body
The body feels the effects of not having enough cortisol and aldosterone. It can affect how you feel, like your energy and stress levels. It also impacts your immune system.
Aldosterone helps control sodium and potassium levels. Without enough, blood pressure can drop too low or rise too high. This can cause serious problems with blood pressure and electrolyte balance.
| Function | Effect of Addison’s Disease |
|---|---|
| Cortisol Production | Decreased stress tolerance, fatigue, and immune suppression |
| Aldosterone Production | Abnormal blood pressure, salt cravings, and irregular heartbeat |
| Metabolic Regulation | Weight loss, reduced muscle mass, and low blood sugar levels |
Exploring the Causes of Addison’s Disease
Addison’s disease is a condition where the adrenal glands are damaged. It can happen for many reasons. The most common reason is autoimmune destruction of the adrenal cortex. This is when the immune system attacks healthy adrenal tissue, stopping it from making hormones.
There’s also a genetic predisposition to Addison’s disease. This means some people might be more likely to get it because of their genes. Families with a history of autoimmune diseases are especially at risk. This shows a link between autoimmune diseases in families.
| Cause of Addison’s Disease | Impact on Adrenal Function |
|---|---|
| Autoimmune destruction | Direct damage leading to hormone deficiency |
| Genetic factors | Increases susceptibility to autoimmune reactions |
| Infections and other diseases | Potential damage or impairment of adrenal glands |
Studies on adrenal gland damage show infections and diseases can harm the adrenal glands. They can either directly damage the glands or trigger autoimmune attacks. This research helps us understand how Addison’s disease starts and grows. It shows the need for more study in genetics and autoimmune diseases.
- Autoimmune triggers
- Hereditary patterns
- Adrenal vulnerability to infections
Knowing about these causes and how they work together is key. It helps us create better treatments for Addison’s disease. These treatments aim to fix the problem, not just the symptoms. This improves care and results for patients.
Identifying Common and Uncommon Symptoms of Addison’s Disease
It’s important to know the symptoms of Addison’s disease early. These signs affect both the body and mind. Spotting them early can help in getting better treatment and improving life quality.
Physical Signs of Addison’s Disease
Physical signs of Addison’s disease can be hard to notice or very obvious. Fatigue, salt craving, and hyperpigmentation are common signs. Fatigue that doesn’t go away with sleep is a big problem. It makes daily tasks hard.
Not being able to balance sodium levels leads to salt craving. This can cause dehydration. Hyperpigmentation makes skin darker, especially where it’s pressed or rubbed.
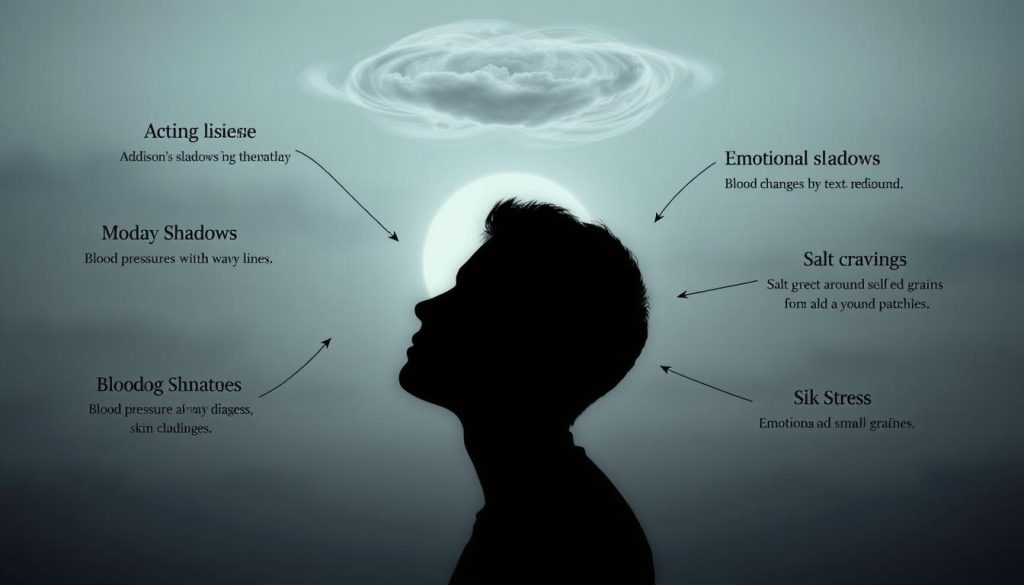
Psychological and Emotional Manifestations
Addison’s disease also affects mental health. Depression is a big concern. The constant fight with symptoms can hurt your mood and mind.
| Common Symptoms | Lesser-Known Symptoms |
|---|---|
| Fatigue | Depression |
| Salt Craving | Low Blood Pressure |
| Hyperpigmentation | Muscle Pain |
Knowing about Addison’s disease symptoms is key. Managing symptoms well can make life better and prevent serious problems. Every symptom is important for treating Addison’s disease fully.
What Is Addison’s Disease: A Closer Look at this Rare Condition
Addison’s disease is a rare condition that affects the adrenal cortex. This part of our body is crucial for hormone production. When it fails, it leads to health problems.

Understanding primary adrenal insufficiency is key. It helps us see how the adrenal cortex works. Addison’s disease shows how important balance in our body is.
| Function | Impact in Addison’s Disease | Normal Condition |
|---|---|---|
| Hormone Production by Adrenal Cortex | Severely decreased | Optimal levels maintained |
| Regulation of Blood Pressure | Potentially life-threatening hypotension | Stable blood pressure |
| Response to Stress | Compromised, leading to potential crisis | Adequate stress response |
| Metabolism of Carbohydrates, Proteins, and Fats | Impaired, affecting overall energy levels | Efficient metabolism supporting energy needs |
| Sodium and Potassium Balance | Disrupted, critical for muscle and nerve function | Well-regulated electrolyte balance |
Studying Addison’s disease highlights the adrenal cortex’s importance. It also shows the wide range of endocrine system disorders. This rare condition can greatly affect our lives, making early diagnosis and treatment crucial.
Comprehensive Diagnosis Procedures for Addison’s Disease
To diagnose Addison’s disease, doctors use blood tests and imaging studies. These tools help confirm the disease, check the adrenal glands’ function, and look for any physical issues.
Blood Tests and Addison’s Diagnosis
The first step is blood tests to check cortisol levels. The ACTH stimulation test is key in this process. It shows how well the adrenal glands respond to ACTH, which is important for cortisol production. A poor response suggests Addison’s disease.
Testing for adrenal autoantibodies in the blood also helps. These autoantibodies show the immune system is attacking the adrenal glands. This attack can make the glands not work right.

Imaging Studies and Other Diagnostic Methods
Imaging studies give a closer look at the adrenal glands and nearby areas. CT scans of the abdomen are especially useful. They show detailed images that can spot structural changes or problems in the glands.
| Diagnostic Method | Purpose | Key Insights |
|---|---|---|
| ACTH Stimulation Test | Assess adrenal response to ACTH | Measures how adrenal glands produce cortisol in response to ACTH |
| Adrenal Autoantibodies Detection | Evidence of autoimmune activity | Indicates immune system’s role in targeting adrenal glands |
| CT Scan | Visual assessment of adrenal glands | Helps identify abnormalities or other structural issues |
By following these diagnostic steps, doctors can accurately diagnose Addison’s disease. This ensures the right treatment is started quickly to manage the disease well.
Potential Treatments for Managing Addison’s Disease
Managing Addison’s disease requires personalized medical care. This care focuses on the hormonal shortages seen in this condition. Hormone replacement therapies are key, helping to make up for the missing hormones from the adrenal glands.
Hormone Replacement Therapies
Glucocorticoid therapy and mineralocorticoid supplements are common treatments. They replace cortisol and aldosterone, crucial hormones. These hormones help with metabolism, immune response, and stress.
Doctors use hydrocortisone, prednisone, and dexamethasone for glucocorticoid therapy. It’s important to adjust the doses carefully. This ensures the hormones are replaced without causing harm.
Mineralocorticoid supplements, like fludrocortisone acetate, are also used. They help keep blood pressure and electrolyte levels balanced. This is vital for the body’s health.
Addressing Acute Adrenal Crisis
An acute adrenal crisis is a serious situation that needs quick treatment. It happens when the body faces extreme stress, like infections or injuries. Symptoms include severe fatigue, dehydration, and low blood pressure.
Emergency care involves giving high doses of glucocorticoids and saline solutions. This helps restore hormone and fluid levels. Glucose is also given to treat low blood sugar. Close monitoring and adjustments are essential to save the patient.
Prognosis of Addison’s Disease: What Patients Can Expect
Knowing about the Addison’s disease prognosis and managing it well is key to a better life. This part will talk about what people with this disease can look forward to. It will focus on the importance of good chronic condition management and other key factors.
Long-Term Outlook for Addison’s Patients
For those with Addison’s disease, the outlook is mostly good with the right treatment and lifestyle changes. The main goal is to replace the hormones the adrenal glands can’t make. With regular treatment, many people live active, full lives. But, they must accept ongoing medication and regular doctor visits as part of their daily life.
Factors Influencing Addison’s Disease Prognosis
Many things can affect how well someone with Addison’s disease does, from genetics to how well they follow their treatment. Here’s a detailed table showing these factors and their effects.
| Factor | Impact on Prognosis |
|---|---|
| Genetic Predisposition | May make people more likely to have autoimmune issues, making the disease harder to manage. |
| Adherence to Treatment | Very important to avoid serious problems; not following treatment can lead to serious issues and shorten life. |
| Accessibility to Healthcare | Seeing doctors regularly helps keep treatment on track, leading to better results. |
| Lifestyle Factors | What you eat, how you handle stress, and your overall health play a big role in managing the disease. |
Lifestyle Changes and Management Strategies for Addison’s Disease
Managing Addison’s disease well needs a full plan. This includes stress management in Addison’s disease, dietary modifications, and adrenal insufficiency education. These steps help patients and their families manage the disease every day and spot any big problems early.
Handling stress is key for Addison’s disease patients. Too much stress can make symptoms worse and even cause life-threatening crises. Using methods like meditation, relaxation, and mental health checks can help keep stress down.
Changing what you eat is also important. Eating the right amounts of sodium, potassium, and carbs helps since the body can’t do it on its own. Working with a nutrition expert to create a special diet is a good idea.
Learning about adrenal insufficiency is crucial. Both patients and their families need to know how the disease works. This includes knowing the signs of a crisis and when to get help fast.
| Management Strategy | Description | Benefits |
|---|---|---|
| Stress Management | Includes techniques like meditation and therapy | Reduces risk of adrenal crises triggered by stress |
| Dietary Adjustments | Balance of sodium, potassium, and carbohydrates | Helps in regulating vital body functions |
| Education | Understanding symptoms and emergency protocols | Empowers patients and caregivers in managing the disease |
Using these strategies can really improve life for those with this chronic illness. By focusing on stress, diet, and education, patients can live more fully and manage their disease better.
Conclusion
Understanding Addison’s disease is key to managing it well. It affects health in many ways and has specific symptoms and treatments. People with this condition need caring guidance and accurate info.
This article aims to make the complex world of Addison’s disease easier to navigate. It helps patients take charge of their health and well-being.
Living with Addison’s disease doesn’t mean you’re alone. Support is crucial for those dealing with it. It connects medical advice with everyday life.
Being part of a community of experts and others with Addison’s disease is important. It shows the value of community in addition to medical care. This support helps people find comfort and strength.
Managing Addison’s disease is more than just medical treatment. It’s about a caring approach that understands the struggles of patients and their families. We hope this information helps build resilience and supports ongoing research into this rare condition.
FAQ
Q: What is Addison’s disease?
A: Addison’s disease is a rare condition where the adrenal glands don’t make enough hormones. These hormones, like cortisol and aldosterone, are crucial for our body’s functions. Without them, we can feel very weak and tired.
Q: How does Addison’s disease affect the body?
A: This disease messes with our body’s balance. It affects how we handle stress, our immune system, and blood pressure. Without enough cortisol and aldosterone, we might feel very weak and tired.
Q: What are the causes of Addison’s disease?
A: Most often, it’s because our body attacks the adrenal glands. Other reasons include infections, genetic issues, and injuries. Scientists are still learning more about what causes it.
Q: What are the symptoms of Addison’s disease?
A: Symptoms come on slowly. You might feel very tired, weak, and lose weight. You could also crave salt, have dark skin patches, and feel sick to your stomach. It can also make you feel depressed or irritable.
Q: How is Addison’s disease diagnosed?
A: Doctors check your symptoms and do blood tests. They look for cortisol levels and check for antibodies. Sometimes, they use CT scans to see the adrenal glands.
Q: What treatments are available for Addison’s disease?
A: Treatment usually means taking hormones to replace what’s missing. You’ll need glucocorticoids for cortisol and mineralocorticoids for aldosterone. If you have a severe crisis, you need to see a doctor right away.
Q: Can someone with Addison’s disease lead a normal life?
A: Yes, with the right treatment and care, you can live a normal life. It’s important to follow your treatment plan and make healthy lifestyle choices. With good care, you can manage your condition well.
Q: What lifestyle changes are recommended for someone with Addison’s disease?
A: To manage your disease, eat well, manage stress, and know your condition. Carry important medical info with you. Regular check-ups with your doctor are also key.
Q: How does stress affect someone with Addison’s disease?
A: Stress is hard for people with Addison’s because they can’t make enough cortisol. This can make symptoms worse or even lead to a crisis. You need to see a doctor right away if this happens.
Q: Is there current research on Addison’s disease?
A: Yes, there’s ongoing research. Scientists are trying to understand the disease better, find better tests, and treatments. They also want to know more about genetics and long-term health.